IAHP
THERAPY:
The most important principle is that
the brain grows by use brain growth and development can
be slowed down or stopped by brain injury, BUT it can also
be speeded up (plasticity of the brain). Everything that we
learn, is learnt through the five sensory pathways into the
brain seeing, hearing, feeling, taste and smell. Brain
injury creates a "barrier" between the environment and
the brain, and a normal stimulus or input (enough for a well
child to develop in all facets) will not get through to an
injured brain.
Therefore the frequency (how often
during the day you do each activity), intensity (how bright
the light in visual stimulus, how loud the sound in auditory
stimulus, how far does the child move in mobility, etc) and
duration (the length of time you do each activity) has to be
high enough, otherwise the message will not arrive in the
brain. With 60 years of experience in treating brain injured
children, the Institutes know exactly at what intensity,
frequency and duration each part of the program has to be
done, for the children to progress. The brain injured child's
capabilities are evaluated in the
three most important input pathways (seeing, hearing and
feeling) and the output pathways (mobility, language and
manual competence). (See the
Institutes developmental Profile at http://www.iahp.org/developmental_profile/index.html
)
A program is then designed and taught
to the parents which helps the child develop
from one stage to another in each pathway through activities
which reinforce the level that the
child is at, and stimulate the next level.
Excellent nutrition, eliminating
harmful chemicals (purifying water and air),
respiratory programs to increase the oxygen supply, and
intellectual programs (reading,
maths and intelligence bits) are vital ingredients of the Institutesı
programs.
The Institutes believe that the
parents are the answer parents know their kids the best
and love them unconditionally and are willing and capable of
working with their kids for many hours daily until their
child reaches its true potential.
Gerard's program has included:
I will only describe Gerardıs program
in general terms, because each program has to be taught to
the parents by the IAHP staff. The program changes as the
child develops.
Vision:
a) Stimulating the light reflex with a
flash light
b) To create outline perception:
Environment around him with checkerboard wall; showing him
black and white outline bits
c) To learn to see detail: Colorful
shapes on checkerboard; detail bits with color
Hearing:
a) Banging two wooden blocks together
b) Other loud noises, like banging
pots and pans, sirens, whistles, etc.
c) Environmental sounds, for example
bells, clapping hands, telephone ringing, musical
instruments
d) Transient Electronic Auditory
Stimulation based on the work of Guy Bérard, TEAS are
CDıs with music on it, interspersed with powerful,
short-duration, random, high-frequency pulses.
Tactility:
a) Contrasting stimulation of hot and
cold; stimulating with sharp fingernails
b) Contrasting stimulation of rough
and smooth
Mobility:
a) Cross-Patterning: Three adults move
the childıs limbs and head through
the movements of crawling or creeping.
The child lies on his tummy on a table. This is not physical
exercise for the child, it is a sensory experience, telling
the childıs brain "This is how it feels to creep"
b) The Floor as a Way of Life:
Spending every available moment on the floor on his tummy.
c) Belly-crawling on a smooth surface
wearing an anti-roll device. Log-rolling is a dead-end in
mobility development, it doesnıt lead to the next stage of
mobility, creeping the anti-roll device prevents the
child from rolling over. He learns that if he wants to move,
he must crawl.
d) Crawling on carpet.
e) Medullary Reflex Program rolling
down an incline.
f) Body Weight Suspension Program
hanging upside down. Gravity helps to stretch his shortened
tendons, improve scoliosis and hip luxation.
g) Assisted creeping with an anti-sit
device on Two adults move his arms and legs in
cross-pattern creeping; the anti-sit device supports his
legs.
h) Creeping on all fours in the
Gravity-Assisted Environment: The child is given the
opportunity to FEEL what it feels like to move using his own
brain and balance areas of his brain. He wears a harness, to
which are fastened bungee cords that come down from a track
attached to the ceiling. He is put in the quad position with
four cords attached to his shoulders and hips.
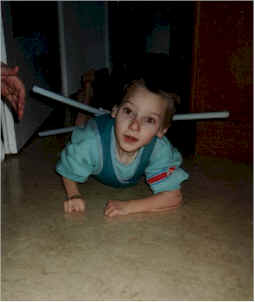
Gerard wearing his anti-roll device
Respiratory Programs:
a) Reflex mask
b) Positive Respiratory Machine
c) Oxygen Enrichment Program
NB: The respiratory programs can and
should only be done when they are prescribed by IAHP, as
there are some contra-indications.
Nutrition:
No sugar in any form; no milk
products; very little salt, liquid balance; a healthy
balance between proteins, carbohydrates and fats in every
meal; vitamin and mineral supplements. For the last 6 months
all the foods that he is allergic to has been taken out of
his diet.
Update Reports
Progress since starting the IAHP
program in May 2000
Mobility: After 8 months on the
program, he reached his belly-crawling goal of 300 metres
per day on the smooth surface. He then started crawling on
the carpet (which is a lot more strenuous, as there is more
friction), and reached his carpet crawling goal of 300
meters per day on 2 December 2001, 19 months after starting
the program. He can now push himself up into a quad position
on all fours, and hold it for 4 minutes. He is well on his
way to learning to creep on all fours. His strength, balance
and stamina has increased vastly. He can crawl 25 meters in
one go. I am 100% convinced that he will learn to walk with
time, based on the many children that I have seen at IAHP
who have made the same mobility progress as Gerard.
Vision: After 2 months on the program,
Gerard could track objects accurately and fast. After
another 2 months, he started seeing detail, which means that
he could see facial expressions and mimic them. He can now
see tiny objects on the floor (as small as a piece of
fluff), crawl to them and pick them up. His nystagmus has
completely disappeared. His strabismus has improved he is
alternating much faster between his eyes. He crawls to
stairs, sees that they are going down, and will stop before
the stairs.
Hearing: This is the area of least
progress. He reacts much more often to sounds (turns his
head towards the sound), but does not do this all the time.
Tactility: After 3 months on the
program, he reacted properly to pain, hot and cold, pulling
away from the stimulation. He can now feel and react to
gentle touch all over his body.
Speech: The volume of his babbling has
increased 10 times. He hardly ever cried, now he lets us
know when he is unhappy or has hurt himself! He is making
many more sounds much more frequently, but his speech
development is dependent on his hearing. He will have to
hear better before he will be able to improve his speech.
Manual competence: He has not yet
developed a pincer grip (grabbing objects between thumb and
index finger), but he can grab objects much faster, hold
them for a long time, deliberately let go of objects, bang
two sticks together.
Weight: In the first year of program,
he put on 1,5 kg, and then stayed at this weight, despite a
high calorie diet of 1 500 calories per day. We had every
conceivable conventional test done (stool, allergy, thyroid,
growth hormone tests), but every test came back negative. In
October 2001, the nutritionist at IAHP did a kinesiology
muscle test, and found several foods and environmental
substances that he was allergic too. From the moment that we
cut out the foods that he was allergic too, he started
eating really well, had no more reflux, and put on 1 kg in
one month!
General: Within one month of starting
the program, his feet were almost straight and had a lot
more tone. The rigidity in his hands and arms have improved
a lot, his left hand (the hand he uses the most) is
beautifully loose. The rigidity in his hips and legs have
improved tremendously. His legs are now nearly straight, his
legs can be opened to an angle of 90° (before program
30°). He has finally realized that he has legs and that
they can be used! He can now swallow liquids without
choking. Feeding him is a pleasure, previously half the food
fell out of his mouth. He is now using his tongue to move
the food to the back of his throat. He knows the members of
his family he gets very upset and starts crying when one
of us leaves the room and leaves him alone. His legs used to
look like sticks, he had no noticeable muscles now he was
super-duper thigh, tummy, back and arm muscles. When we pick
him up, he grabs us round the neck to give us a hug.
He can be held upright just by holding
him under his bottom previously he would have flopped
backwards immediately. According to IAHPıs evaluation in
October 2001, he has progressed 9 times faster in the 1,5
years that he has been on the program, compared to the
entire 4,5 years before he started the program.
March 2004:
Gerard finally started hearing after 3 years of program - he
can now hear and understand everything. He is
communicating with us using a facilitated communication
board. He facilitates in 3 languages (Afrikaans, English and
German), spelling out sentences on the communication board.
He can read very well at a 12 year old level - print size is
8 mm. He can push himself up into a quad position and is
creeping short distances (up to 3 meters non-stop) on all
fours. He can sit in a W-position, supporting himself on one
hand, using the other hand to do manual tasks. He is making
many new sounds, but no language yet.
Why has he progressed so much faster
with the intensive IAHP program?:
First of all, the other therapies were
not intensive enough in terms of time to make a real
difference for a profoundly brain-injured child like Gerard.
Secondly, each therapy program that we
pursued addressed only one specific area of his development.
For example, Bobarth-therapy is a neurologically-based
physiotherapy, but because he did not spend enough time on
the floor on his tummy, his mobility development was much
too slow.
Without solving the problem of
increasing spasticity, his mobility development would have
slowed down even more, and he would probably have regressed.
The Institutes' program addresses
every area of development in a structured way. Everything is
interdependent if the child canıt see well enough, he is
not motivated to move. If he canıt feel where his leg is,
he can't move.
If his breathing is inadequate, he has
no stamina to move. If his nutrition is bad, his brain and
body is not getting the nutrients it needs to function
properly. If he is too thin, he has no stamina to move
enough to be able to get to the next stage in mobility
development, etc. On the other hand, every bit of progress
in any area has a positive influence on the other areas.
I have been amazed at his progress in
the last year and 10 months, and look forward to his further
development he has not nearly reached his true potential.
Contacts:
The Institutes for the Achievement of
Human Potential: http://www.iahp.org/